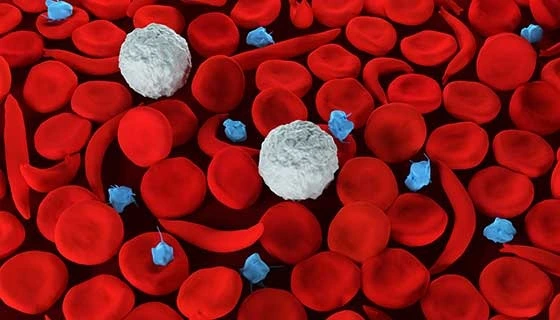
Sickle Cell Disease: Causes, Symptoms, and Advances in Treatment .A collection of hereditary blood illnesses known as sickle cell disease (SCD) are distinguished by the presence of hemoglobin S, an aberrant form of hemoglobin. This abnormality leads to the distortion of red blood cells into a sickle or crescent shape, impairing their ability to transport oxygen efficiently throughout the body. The disease manifests in various forms, with sickle cell anemia being the most prevalent. Globally, SCD affects millions, with a significant concentration in sub-Saharan Africa, India, the Middle East, and among individuals of African descent in the United States.
Genetic Basis and Inheritance
A mutation in the HBB gene, which codes for hemoglobin’s beta-globin component, results in sickle cell disease. This mutation results in the substitution of the amino acid valine for glutamic acid at the sixth position of the beta-globin chain. The disease follows an autosomal recessive inheritance pattern, meaning an individual must inherit two copies of the mutated gene (one from each parent) to exhibit the disease. Individuals with only one copy of the mutated gene are carriers, known as having sickle cell trait, and typically do not display symptoms but can pass the gene to their offspring.
Pathophysiology
Under low oxygen conditions, the abnormal hemoglobin S polymerizes, causing red blood cells to become rigid and adopt a sickle shape. These deformed cells are less flexible and can obstruct small blood vessels, leading to impaired blood flow and oxygen delivery to tissues. This vascular occlusion is responsible for many of the disease’s complications, including pain crises and organ damage. Additionally, sickled red blood cells have a reduced lifespan, leading to hemolytic anemia.
Clinical Manifestations
The symptoms of SCD typically emerge around five to six months of age and can vary in severity. Common manifestations include:
- Anemia: Due to the rapid destruction of sickled red blood cells, individuals often experience chronic fatigue and pallor.
- Pain Episodes (Vaso-occlusive Crises): Periodic episodes of severe pain occur when sickled cells block blood flow to bones, chest, and joints. These crises can last from hours to days and may require hospitalization.
- Swelling of Hands and Feet (Dactylitis): Painful swelling results from blocked blood circulation in the extremities.
- Frequent Infections: Damage to the spleen impairs the body’s ability to fight infections, increasing susceptibility, particularly in children.
- Delayed Growth and Puberty: Chronic anemia can lead to delayed growth in children and delayed onset of puberty.
- Vision Problems: Blockage of tiny blood vessels supplying the eyes can lead to retinal damage and vision issues.
Complications
SCD can lead to various severe complications, including:
- Stroke: Blocked blood flow to the brain can result in a stroke, leading to permanent neurological damage.
- Acute Chest Syndrome: Characterized by chest pain, fever, and difficulty breathing, this condition is caused by sickling in the lungs and can be life-threatening.
- Organ Damage: Chronic deprivation of oxygen can damage organs such as the kidneys, liver, and heart.
- Leg Ulcers: Poor circulation can lead to chronic, non-healing sores on the legs.
Diagnosis
Early diagnosis is crucial for managing SCD effectively. In many countries, newborn screening programs test for SCD using blood tests that detect the presence of hemoglobin S. Prenatal testing is also available for at-risk pregnancies through procedures like amniocentesis or chorionic villus sampling.
Management and Treatment
While there is no universal cure for SCD, several treatments can alleviate symptoms and prevent complications:
- Medications: Hydroxyurea is commonly prescribed to reduce the frequency of pain crises and acute chest syndrome. It works by increasing the production of fetal hemoglobin, which prevents the formation of sickle cells.
- Blood Transfusions: Regular transfusions can increase the number of normal red blood cells, reducing the risk of stroke and other complications.
- Bone Marrow Transplant: Also known as stem cell transplant, this procedure offers the potential for a cure but is typically reserved for severe cases due to associated risks.
- Preventive Measures: Vaccinations and prophylactic antibiotics are essential to prevent infections. Patients are also advised to stay hydrated, avoid extreme temperatures, and manage stress to reduce the risk of pain crises.
Recent Advances
Advancements in gene therapy offer promising avenues for curing SCD. Techniques like CRISPR-Cas9 are being explored to correct the genetic mutation responsible for the disease, potentially providing a definitive cure in the future.
Living with Sickle Cell Disease
Managing SCD requires a comprehensive approach that includes regular medical care, lifestyle modifications, and psychosocial support. Patient education is vital to empower individuals to recognize symptoms early and seek appropriate care. Support groups and counseling can also play a significant role in improving the quality of life for patients and their families.
For more detailed information on Sickle Cell Disease, including symptoms, causes, and treatment options, you can refer to the Mayo Clinic’s comprehensive guide.
In conclusion, while Sickle Cell Disease presents significant health challenges, ongoing research and improved management strategies continue to enhance patient outcomes. Early diagnosis, proactive management, and staying informed about new treatment options are crucial steps in managing this condition effectively.
